Preparedness is not a health expense—it is economic infrastructure.
Edwin Shumba,
LabVoice Issue 02
In March 2021, a doctor in a Nairobi hospital faced a wall of silence. Her patients were falling ill with unprecedented speed, but the samples sat waiting, destined for a sequencing lab thousands of miles away in Europe and in the United States.
Africa’s defence against the Covid -19 pandemic was hampered by a fragmented truth: we could not fully see the enemy. This was the cost of limited genomic sovereignty.
The Saving Lives and Livelihoods Pathogen Genomics Project was born out of this urgent need. The “why” was clear: without genomic capacity, Africa was blind in a pandemic.
The “how” was a story of partnership—Africa CDC, Africa Society for Laboratory Medicine (ASLM), and global allies came together to turbocharge the Africa Pathogen Genomics Initiative (Africa PGI), wiring a continental nervous system for outbreak response.
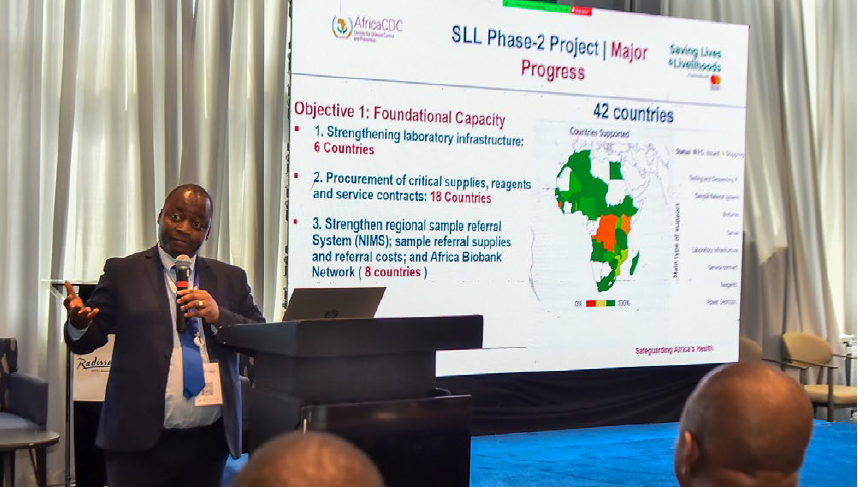
Phase 1 began in June 2022, with only seven countries having Next Generation sequencing (NGS) capacity in National public Health Institutes or equivalent. Today, 46 countries are part of this genomic revolution. This is not just growth; it is continental transformation.
This is the truth: A continent that can identify a threat within its own borders cannot have its diagnostics held hostage by supply chains 8,000 miles away.
What did this leap build?
The Hardware of Sovereignty: Biobanking systems in eight regional hubs; sequencing machines for 20 nations; reagents for 45 labs; and bioinformatics engines in 26 countries. Even local vaccine production at The South African Health Products Regulatory Authority (SAHPRA) gained crucial support.
The Human Code: In Senegal and Kenya, 171 professionals from 35 countries became genomic sentinels, mastering the language of pathogens. Hands-on training in genomic sequencing and Bioinformatics was provided at the centers of excellence across the continent. How was this achieved?
The Integrity of Data: External Quality Assurance moved us from guesswork to guarantee. 577 labs achieved a 92.5% pass rate in polymerase chain reaction (PCR) testing—a bedrock of trust.
The Architecture of Coordination: The African Pathogen Genomics Surveillance Policy Framework and Network Information Management System (NIMS) sample referral system mean we no longer fight in the dark.
The Architecture of Data Sharing: The launch of AGARI (Africa Genomic Archive for Response & Insights)—Africa’s first genomic data-sharing platform—cements our ability to turn raw data into actionable intelligence.
These are not symbolic wins. They are the immunological synapses of a continent. But this new capacity is a seedling, not yet a deep-rooted tree. Training cannot keep pace with need.
Bioinformatics prowess is concentrated in pockets. As more countries sequence, quality wavers—a stark reminder that capability requires constant calibration.
Most critically, we remain perilously dependent on imported reagents, vulnerable to the next global shock. A temporary pause in activities laid bare the risk of progress built on donor timelines, not domestic mandate.
The genomic sequence that shortens an outbreak by two weeks is worth more than gold. It protects markets, schools, and the very fabric of our societies.
The next chapter is about institutionalisation, not implementation:
Codify the right to see: Make genomic surveillance a legislated public good, funded by permanent budget lines.
Mandate excellence: Annual External Quality Assessment (EQA) participation must be non-negotiable, with public scorecards driving improvement.

Scale the army: Move from ad-hoc workshops to structured fellowships and career pathways. We need hundreds, not dozens.
Secure our tools: Implement pooled procurement, customs waivers, and incentivise regional manufacturing.
Govern data with trust: Domesticate the continental policy framework into national law. Health data is a strategic asset.
The Saving Lives and Livelihoods began as a lifeline in crisis. It has grown into a continental immune system. But momentum is not a destination. The choice is stark: lock these gains into law and budgets—or pay a devastating premium in lives and livelihoods when the next threat emerges.
If we choose wisely, future outbreaks will be shorter, smaller, and less destructive.
This is the ultimate return on investment: not just lives saved today, but a future where African livelihoods flourish, secured by our own vigilant hands. This is indeed the power of collaboration. Today, Africa’s livelihoods are safer.