The Results Are In: How a National Sample and Results Transport Network is Improving Patient Care in Uganda
The Results Are In: How a National Sample and Results Transport Network is Improving Patient Care in Uganda
Two of the greatest challenges a laboratory network faces when tackling high-risk global health security threats is the safe transportation of a potentially bio-hazardous specimen and the length of the waiting process for test results. To combat this, we must look to innovative approaches for the efficient transportation of samples and test results through integrated and highly centralised laboratory networks. Ultimately, the goal is a substantial reduction in time during that crucial window where urgent care is critical to the individual patient and the containment of the health security threat.
Laboratory networks, such as the African Public Health Laboratories Network (APHLN), have been looking at specific approaches to accelerate sample and test result delivery that can be applied on regional or international levels. Uganda has shown particular success in this area, beginning with steps taken by the Ugandan Ministry of Health in 2006 to implement Early HIV Infant Diagnosis (EID) testing. Previously, laboratories in Uganda had relied on the country’s major courier provider (Posta Uganda), to deliver samples and results between health facilities and laboratories. But this system was flawed, serving only the 35% of facilities that were located in urban areas along the postal delivery routes [1]. In some cases, trained health professionals themselves were tasked with bringing samples to be tested, not only inconveniencing them, but depriving patients of care while they were gone from their posts. The system, in addition to being prohibitively expensive, resulted in long result turn-around time and was therefore detrimental to patients’ access to care, as their conditions were liable to worsen in that lengthy span of time.
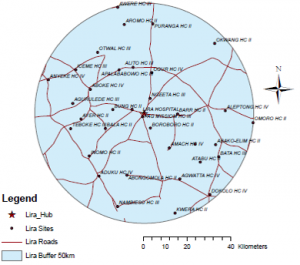
The network’s success relies heavily on connecting lower-level community laboratories, which lack the capacity to run high-level diagnostic testing services, with the better-equipped hubs. By combining the extensive reach of the hubs to the lower-level laboratories, patients across the country have greater access to EID, CD4, HIV viral load, and a number of other specialised tests, resulting in a standardised and elevated level of care. In a comprehensive study on the effects of NSRTN on EID testing in Uganda, researchers determined that the network reduced both the time and cost of sample and result transportation and increased the total volume of tests that could be performed [1].
According to Director General of Health Services, Dr. Jane Ruth Aceng, “the NSRTN has vastly expanded the services patients receive in Uganda, particularly in rural communities where transportation had been a particular challenge. Now patients in all corners of the country are connected to the same high-level of care.”
“It is hopeful that the success of Uganda’s sample transportation network can be duplicated in other countries with the potential for much wider application across the continent. Implementation of such networks is primarily contingent on the support of a country’s Ministry of Health in making, sometimes dramatic, changes in current operations,” says Mah-Sere Keita, ASLM Director of Global Health Security. “Once initial buy-in and support is made, connecting laboratory networks through transport systems can lower costs and improve patient care, making the changes well worth it for governments and the well-being of their people.”
By: Sam Donnenberg; Contributor: Charles Kiyaga; Editors: Michele Merkel, Corey White, Mah-Sere Keita
[1] Uganda’s New National Laboratory Sample Transport System: A Successful Model for Improving Access to Diagnostic Services for Early Infant HIV Diagnosis and Other Programs. C Kiyaga et al. PLoSOne 8(11): e78609, 13 November 2013. Accessed on 9 December 2015: http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0078609
[2] Uganda’s Specimen and Referral Transport System. Charles Kiyaga. 2012. Accessed on 9 December 2015: https://aslm.org/aslm2012/images/docs/Thursday-December-6th-2012/Oral-Presentations/Laboratory-Clinical%20Interface%20-%20Bridging%20the%20Gap/1.%20Charles.pdf
[3] Interview with Charles Kiyaga, Uganda Ministry of Health and ASLM Country Ambassador, 15 December 2015.

